
How Do You Get Tested for Melanoma
Let’s walk through a scenario where a patient gets tested for melanoma.
Mrs Jones, a lovely 72-year-old retired nurse, presents to the skin doctor because she has had no skin checks for the past 10 years. She was motivated to attend the clinic because her childhood best friend was recently diagnosed with a melanoma on her back. Since they grew up together and spent many summers in their youth on the beach without sunscreen, she is understandably concerned about herself. After all, Mrs Jones is way fairer and has way more freckles than her bestie and she recalled numerous episodes of blistering sunburns.
Step 1: Seeing a doctor for a skin check
Mrs Jones presents to Dr Glo who is a doctor with expertise in performing skin checks. Dr Glo takes a comprehensive history (hyperlink to checklist) to determine her risk factors for skin cancer. After this, Dr Glo obtains consent from Mrs Jones about doing a comprehensive full skin examination which involves her removing all her clothes as well as shoes and socks except her underwear (bra and panties) in a private clinic space.
Dr Glo scans the body closely, looking for any suspicious lesions or skin changes using proper lighting instruments and a handheld device called a dermatoscope to examine suspicious skin lesions under high magnification.
Step 2: During a skin check
If no suspicious lesions identified
If no suspicious lesions have been identified during a skin check, Mrs Jones will be asked to return in 1-2 years for further skin checks as dictated by her risk factors. She will also be asked to return earlier if she detects any new or changing lesion. Ongoing and regular sun protection would be recommended.
PRO TIPS
Find more advice in our “Sun Protective Measures” article.
If suspicious lesion(s) identified
If suspicious lesions are identified on Mrs Jones, Dr Glo will look at the lesion of concern closely with a dermatoscope.
Depending on how suspicious the lesion is, Dr Glo may approach as follow:
Example: Lesion on back.
- Interval monitoring for lesions not highly suspicious for melanoma : For lesions that are not suspicious for melanoma but require close monitoring, Dr Glo will make a record of the lesion in the medical records with photographs and ask Mrs Jones to return within a set period of time for progress monitoring. If the lesion has resolved or is unchanged by next visit, no further steps would be required and the lesion will be reviewed at next routine visit. However, if the lesion fails to resolve by next visit and/or has shown progression or change, then a biopsy would need to be done.
- Immediate biopsy for high suspicious lesions: If the clinical suspicion is high and concerning for a melanoma. Immediate action needs to be taken and a biopsy should be done to confirm the diagnosis of melanoma on the same day. This involves an medical office-based procedure using local anesthetic to remove the lesion in its entirety if practical using various techniques (hyperlink). The tissue is then transported to the laboratory for further processing and analysis under the microscope by a trained pathologist. The pathologist will assess the various characteristics of the melanoma (such as the type, thickness, ulceration and mitotic rate). This information is crucial to determining the subsequent treatment decisions.
Step 3: Awaiting for the results
The results usually take 1-2 weeks to return. During this time, patients are provided with instructions on appropriate wound care. This is understandably a difficult time for patients as it can be quite nerve-wracking to wait for the results to come through.
Step 4: Returning to Dr Glo for results
Mrs Jones returns 2 weeks after the biopsy of the lesion on her back. The biopsy site has healed well and the sutures were removed. Dr Glo has the pathology results printed and goes into the details of the report findings to Mrs Jones. The lesion turned out to be a melanoma:
- Early melanoma detected – An early melanoma with a thickness of 0.2 mm considered as early invasive was detected. The melanoma is classified as an early stage melanoma and the next course of action would be for further wide local excision.
- More advanced melanoma detected – A late stage melanoma was detected and there were concerns about spread of melanoma to distant sites. In which case, further staging such as imaging needs to be done. As well, patients may be referred to other medical specialists including melanoma surgeons, medical oncologists and radiation oncologists to determine whether treatments such as surgery, immunotherapy, targeted therapy, radiation therapy, or a combination of these will be required.
Step 5: Treatment of melanoma
Treatment of melanoma depends entirely on the melanoma characteristics and the stage. The treatment varies quite drastically and it is important to engage your doctor. Early stage melanomas require further excision whilst more advanced stage melanomas require multidisciplinary care with other medical specialities involved.
Step 6: Continued Follow up
Following the diagnosis of melanoma, more frequent follow ups are required particularly within the first 5 years of diagnosis. Please refer to your local guidelines for the recommended scheduling for reviews. Remember, early detection is key.
Also, it is important for patients to adopt sun smart measures such as wearing protective clothing, wearing SPF50+ sunscreens, seeking shade whenever possible and to avoid unnecessary sun exposure.
 Common Skin Conditions
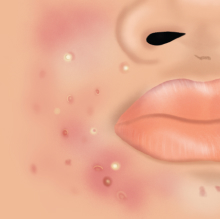
Common Skin Conditions Paediatric Conditions
Paediatric Conditions Skin Cancer
Skin Cancer Infectious Skin Conditions
Infectious Skin Conditions Other Skin Conditions
Other Skin Conditions Treatment & Management
Treatment & Management Prevention & Skincare
Prevention & Skincare











Popular Articles