
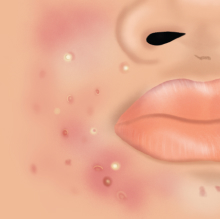
Atopic dermatitis, also known as eczema, is a chronic skin condition that causes itchy, dry and inflamed patches of skin. It is a chronic condition that begins during childhood and continues into adulthood in some.
It is important to treat eczema because of the following reasons:
1. Symptom relief
Itch is a common complaint. It is not uncommon for eczema sufferers to scratch until their skin bleeds. The itch and pain can affect a person’s quality of life such as disturbed sleep.
2. Preventing complications
One of the most common complications of eczema is skin infection due to skin breakdown. It is important to treat this as soon as possible to prevent further complications.
3. Protecting the skin to prevent flare-ups
For patients with eczema, the skin, which acts as a protective barrier, is not working properly. When this barrier is impaired, it becomes weaker and more vulnerable to irritating substances, allergens and moisture loss. It is important to strengthen the skin to prevent flare-ups.
4. Emotional well-being
Patients with eczema can become self-conscious because the appearance and texture of their skin is abnormal. This can cause distress for some. With treatment, the appearance and texture of the skin can improve.
Please find below some recommendations to treat the eczema:
Moisturize with bland, non-fragranced ointments or creams
- Use at least twice daily morning and evening lifelong. Apply more frequently to areas around the mouth and the diaper area in children.
- Moisturize within a few minutes after a bath or shower when the skin is still slightly damp
- Apply moisturizer downwards in the direction of hair growth. DO NOT rub up and down or in circles, as this can cause folliculitis to develop
- Tube based moisturizers are preferred over tub based creams as there is lower risk of bacterial contamination.
- Use bland, fragrance free ointments and creams.
Gentle, soap-free washes (soap substitute)
- Non-fragranced, soap free washes recommended over soaps as the latter tend to dry the skin and can worsen eczema.
Showering or Bathing
- Use warm, rather than hot water.
- Limit showers and baths to 5-10 minutes.
- If taking a bath, a capful of bath oils (non-fragranced), should be added to the bath to soothe the skin.
- Pat the skin dry with a towel after bath. Avoid vigorous rubbing of skin as this can irritate the skin and cause eczema.
Bleach Baths
- Bleach baths are a safe and effective way to keep the skin clear of bacteria which causes skin infections. Bleach baths can be taken during an active infection or up to 3 times a week for several months to prevent the infection from coming back.
EXTENDED READ
Interested in learning more about bleach baths?
Read our in-depth Understanding Bleach Baths: A Step-by-Step Guide for details.
Clothing and Bedding
- Wear lightweight, cotton and breathable clothing.
- Use laundry detergents for sensitive skin and avoid laundry sanitisers.
Antimicrobials
- Antibiotics: Topical or oral antibiotics can be prescribed if there is a bacterial infection. This is generally taken for 7-10 days as prescribed. A skin swab may be taken prior to starting the antibiotics to identify the bacteria causing the skin infection.
- Antivirals: Oral antivirals can be prescribed if there is an infection caused by the cold sore virus. A skin swab may be taken to confirm the viral skin infection.
Topical Corticosteroids Treatment
- During acute flares of eczema, topical corticosteroids are safe to use 1-2 times per day to the entire affected area of skin. It is important to use the appropriate potency of topical corticosteroids prescribed by your healthcare provider. Topical corticosteroids are generally used until the eczema has cleared.
Topical calcineurin inhibitor (tacrolimus)
- Tacrolimus (0.1% in ointment) is a steroid-sparing agent that can be used as long-term treatment of atopic eczema to control and prevent flares. It is often prescribed to be used once a day at night.
 Common Skin Conditions
Common Skin Conditions Paediatric Conditions
Paediatric Conditions Skin Cancer
Skin Cancer Infectious Skin Conditions
Infectious Skin Conditions Other Skin Conditions
Other Skin Conditions Treatment & Management
Treatment & Management Prevention & Skincare
Prevention & Skincare











Popular Articles