Introduction
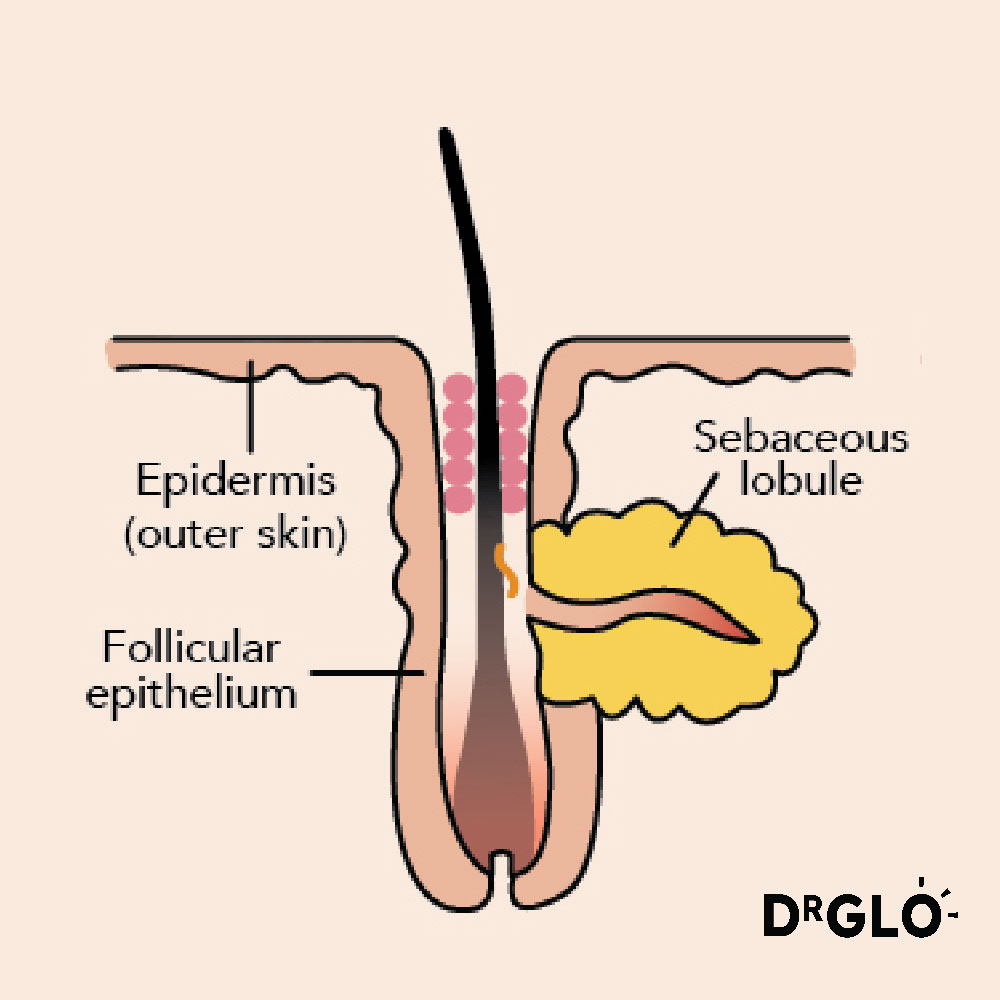
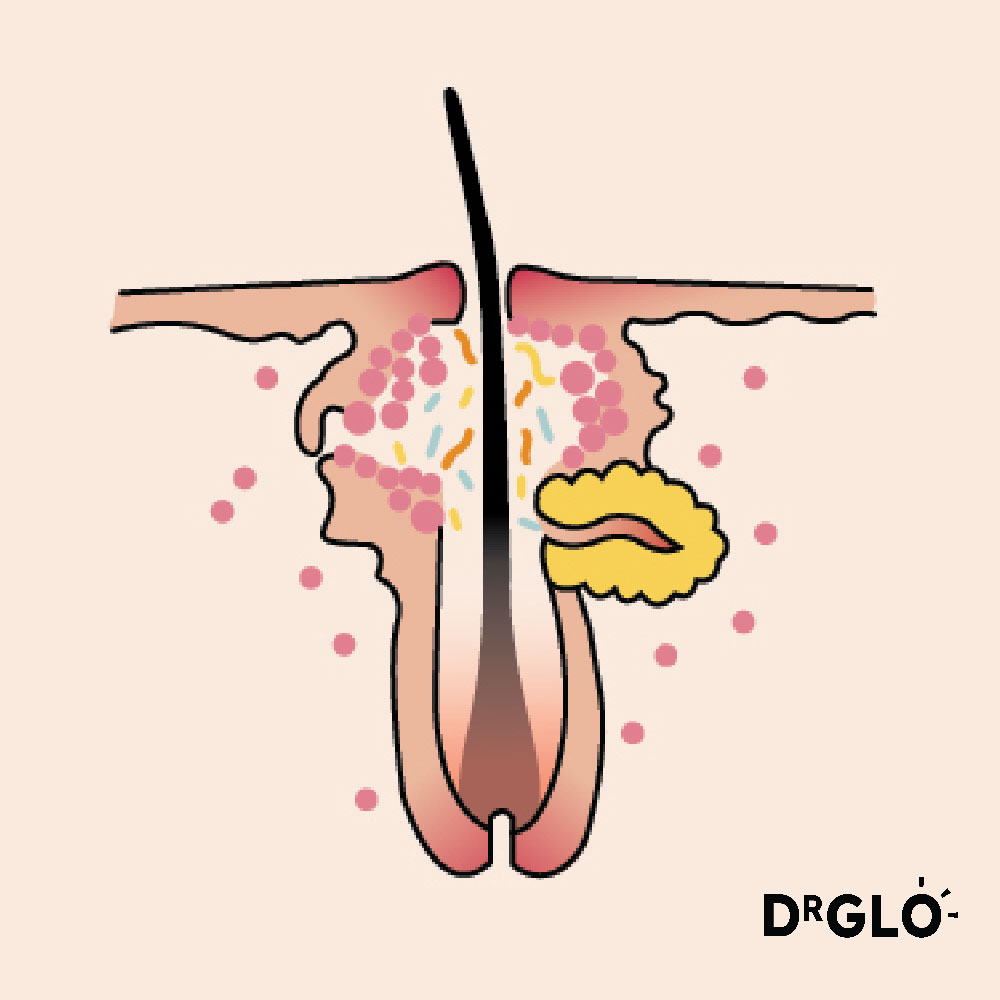
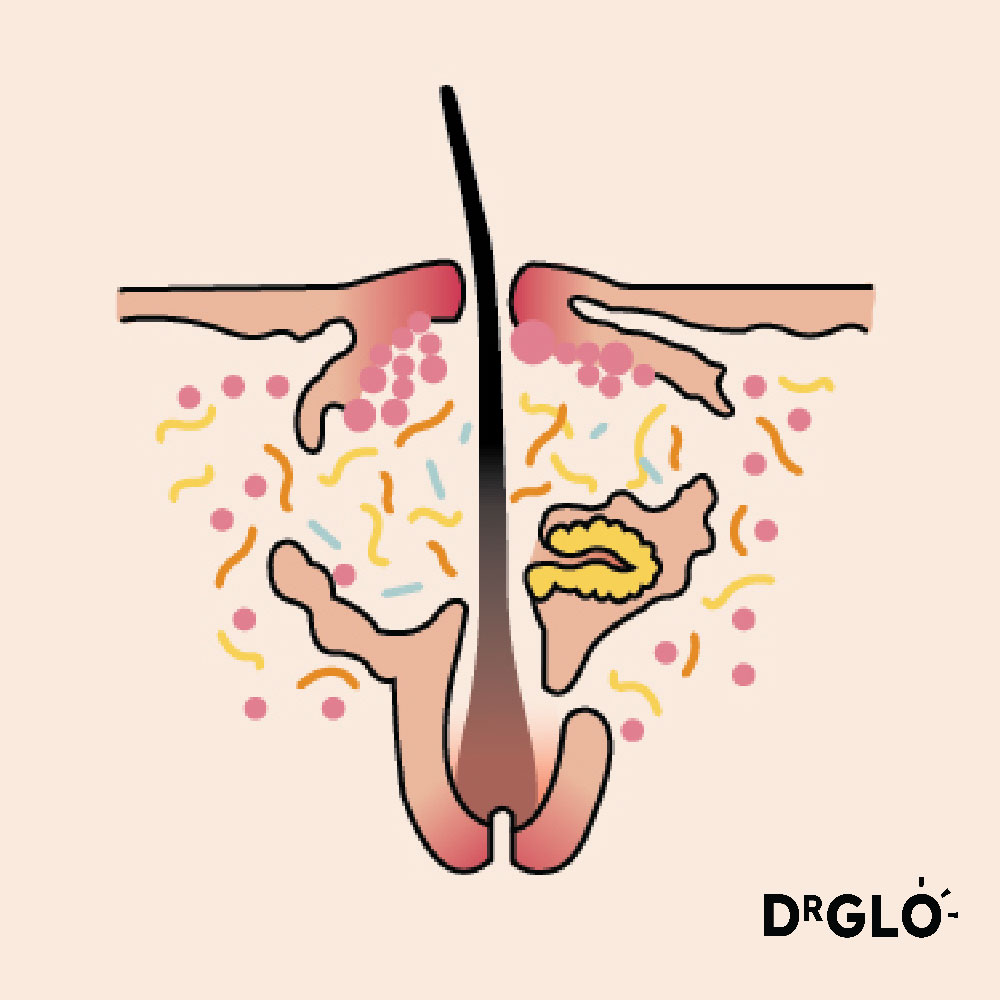
Normal Hair Follicle
Acne vulgaris, commonly known as acne, is a disorder of hair follicles. It is characterized by the presence of various types of lesions, including whiteheads, blackheads, pimples, and cysts. The exact cause of acne vulgaris is not fully understood, but it is believed to involve a combination of factors, including
- excess oil production
- clogged hair follicles
- bacteria (Propionibacterium acnes) on the skin
- Inflammation
Types of acne
The clinical presentation for acne varies depending on severity.
Non-inflammatory Acne – Comedonal Acne
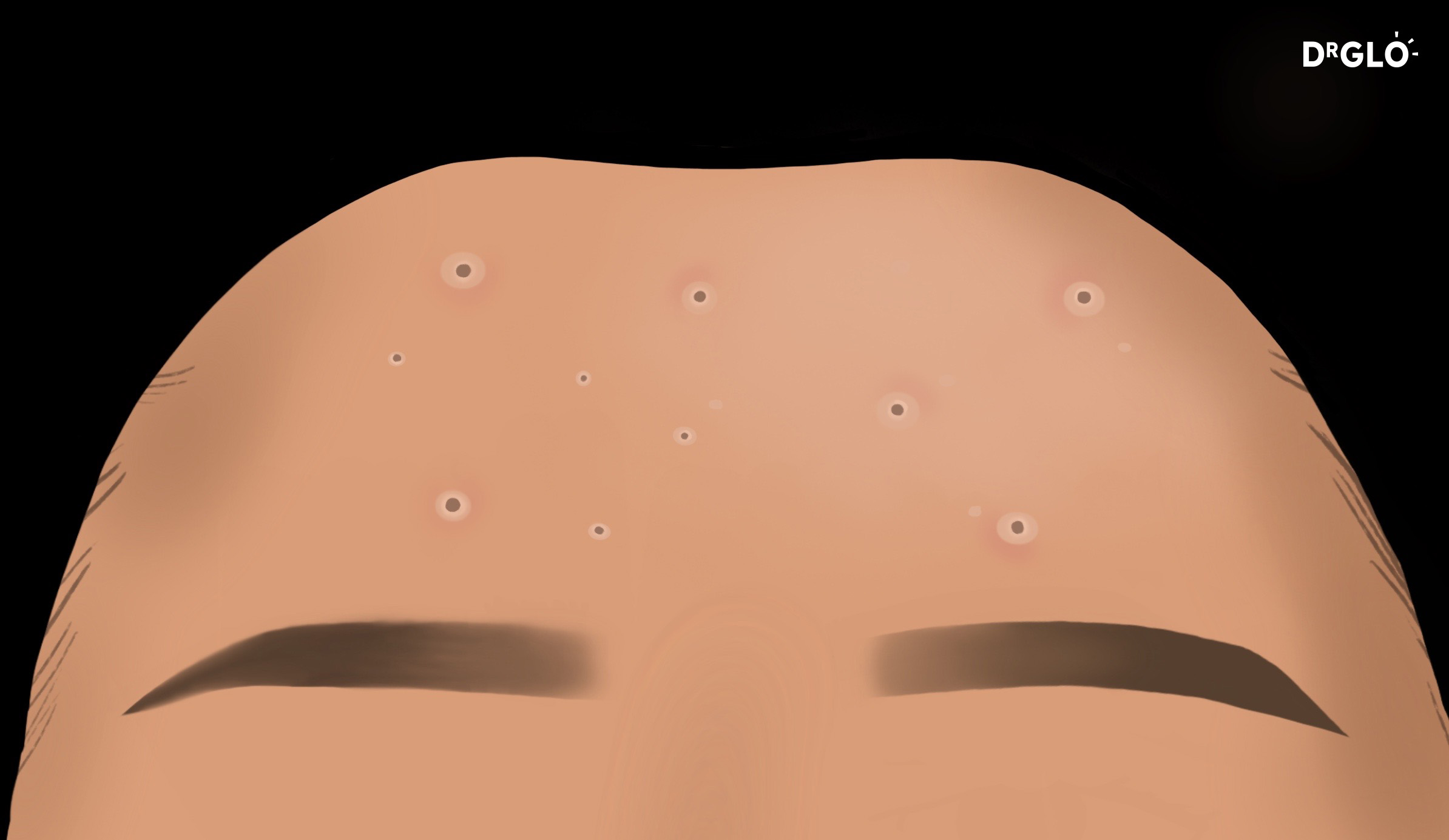
Comedonal Acne
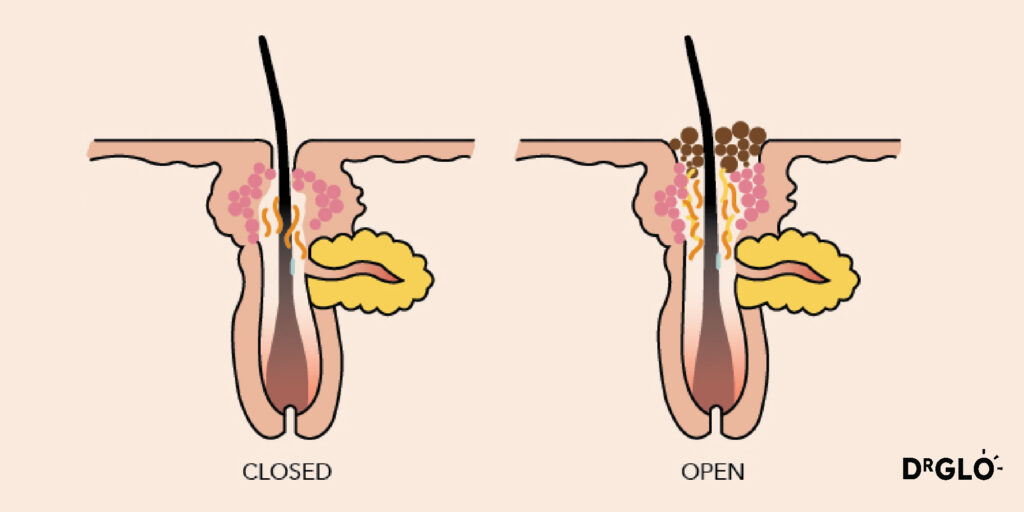
Comedone – Closed and Open Types
These are non-inflammatory lesions and can be of two types:
Whiteheads (closed comedones): Formed when a hair follicle becomes clogged with oil and dead skin cells, causing a white bump to appear on the skin.
Blackheads (open comedones): Formed when a hair follicle opening is widened, and the accumulated material oxidizes, giving it a dark appearance.
Inflammatory Acne – Papulopustular Acne
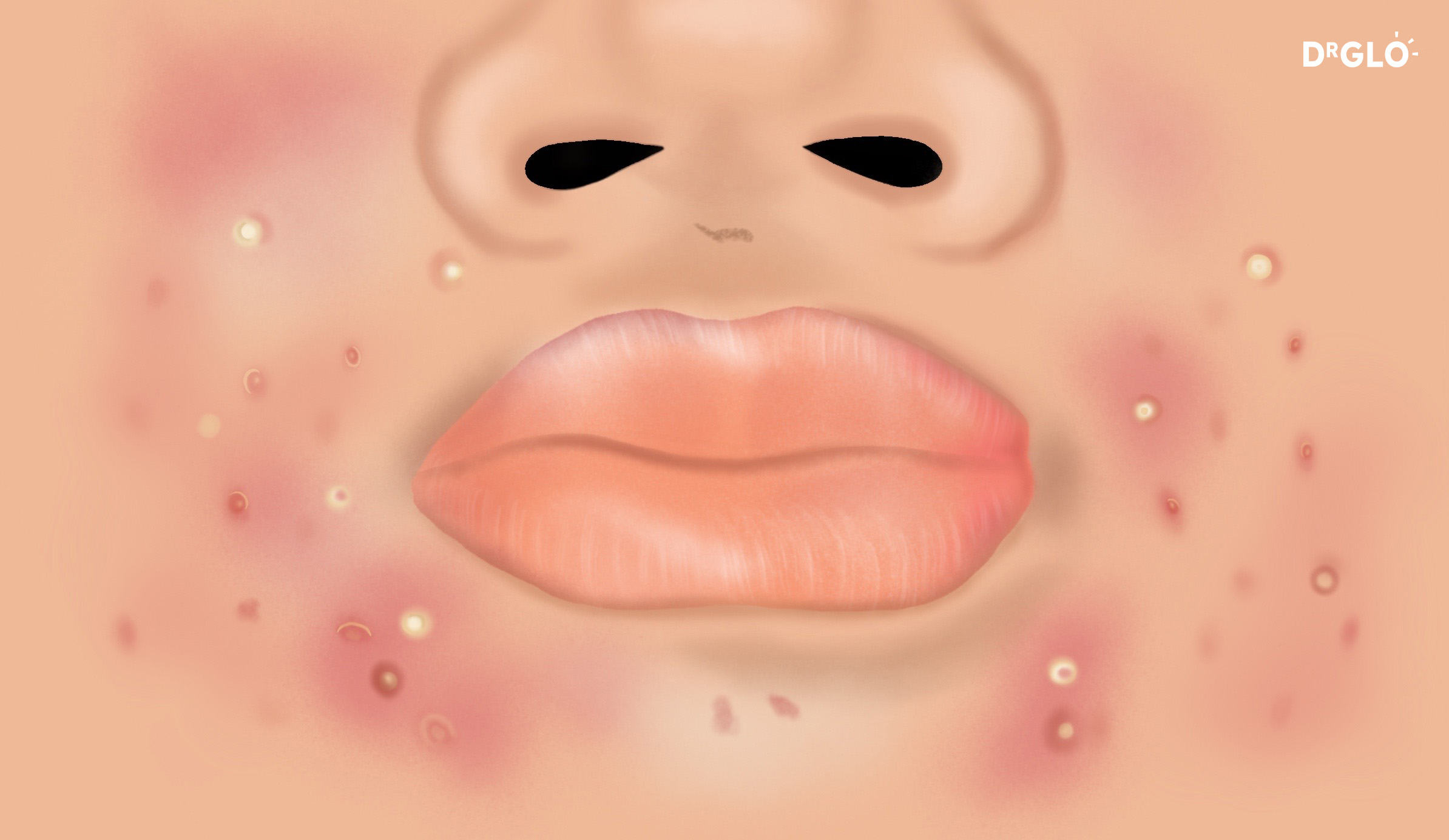
Papulopustular Acne
Inflammatory Papules/ Pustules
These are the result of the immune system’s response to the clogged follicles and bacterial activity.
They can include: Papulopustular acne
- Papules: Small red bumps on the skin.
- Pustules: Pus-filled lesions with a red base.
Inflammatory Acne – Nodulocystic Acne
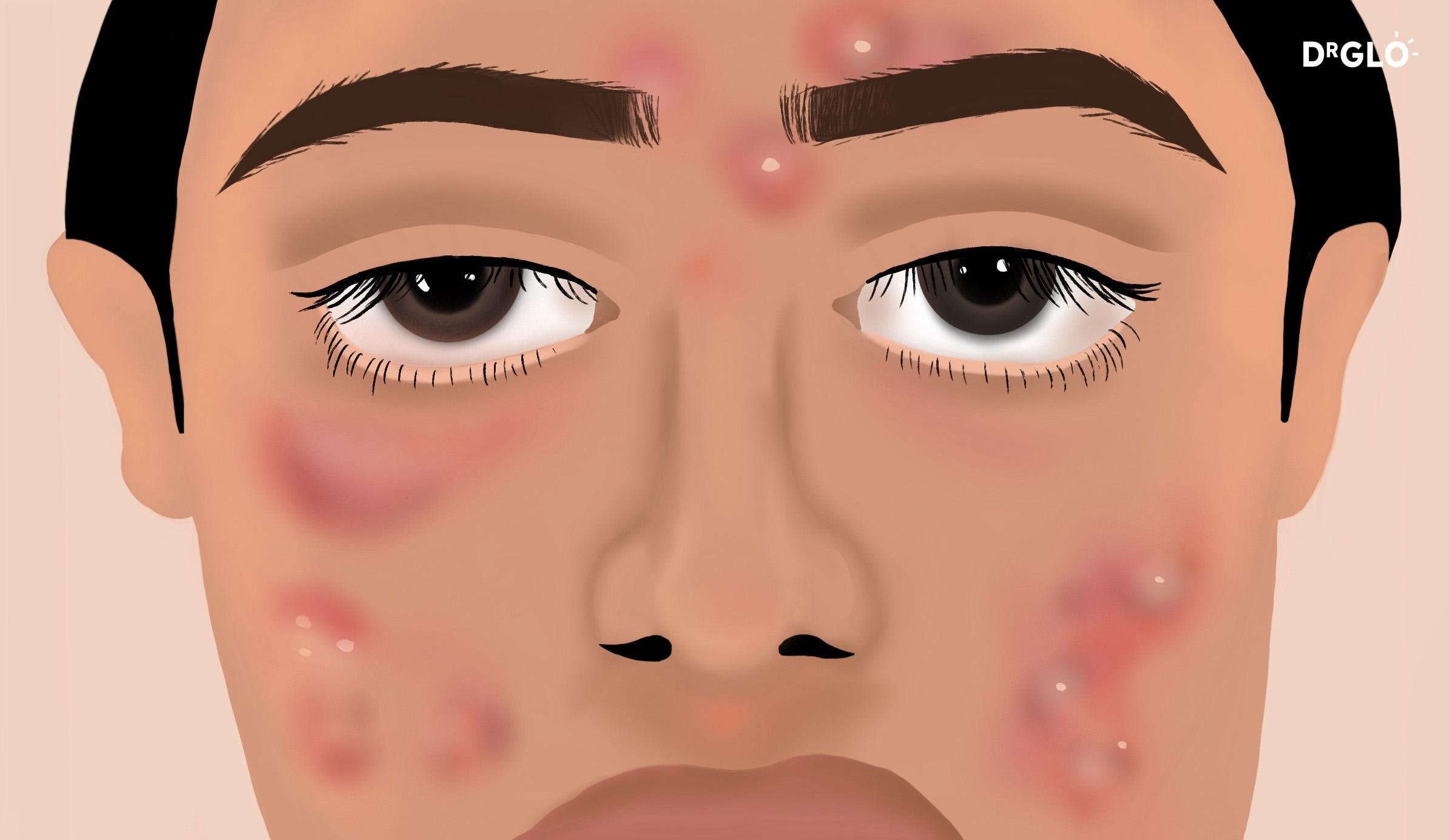
Nodulocystic Acne
Nodule/ Cyst
Nodulocystic acne
- Nodules: Large, painful, solid lesions deep within the skin.
- Cysts: Deep, pus-filled, painful lesions that can cause scarring.
Treatment
Treatment is aimed at addressing the 4 factors involved in acne.
It is important to take into consideration patient factors such as age, biological gender, reproductive plans, underlying medical conditions and compliance with treatment.
Treatment options for acne vulgaris include topical medications (such as benzoyl peroxide, retinoids, and antibiotics), oral medications (such as antibiotics, hormonal therapies, and isotretinoin), and various procedures performed by dermatologists (such as chemical peels, laser therapy, and extraction of lesions). The specific treatment approach depends on the severity of the acne and individual factors.
 Common Skin Conditions
Common Skin Conditions Paediatric Conditions
Paediatric Conditions Skin Cancer
Skin Cancer Infectious Skin Conditions
Infectious Skin Conditions Other Skin Conditions
Other Skin Conditions Treatment & Management
Treatment & Management Prevention & Skincare
Prevention & Skincare